How to Read an Explanation of Benefits (EOB)
If you disagree with how your claim was processed, check out How To Appeal a Claim.
If you receive an EOB with a service subject to the No Surprises Act (NSA), please click here for information related to protection against surprise medical bills. You should not be billed for amounts over your cost-share (your deductible, copay amount, and any coinsurances you may owe).
-
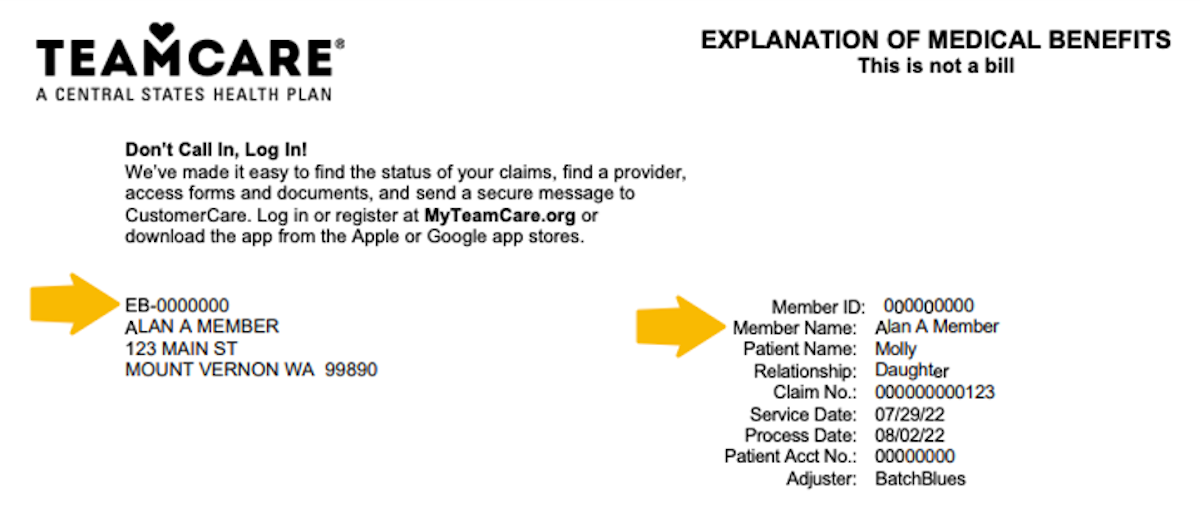 1
1In this section you’ll see who on your plan was treated, and the service date(s).
You’ll also find an assigned claim number to use when referencing your claim, and the time that status was updated.
-
 2
2This is where TeamCare helps you get a complete view of your charges in detail. You’ll find the total billed amount, any amount discounted by TeamCare, and the amount paid for by TeamCare according to your plan’s coverage. In the final box, you’ll see the amount you may still have to pay to the provider.
The next section details the amount this claim has contributed to your annual deductible and out-of-pocket limit.
-
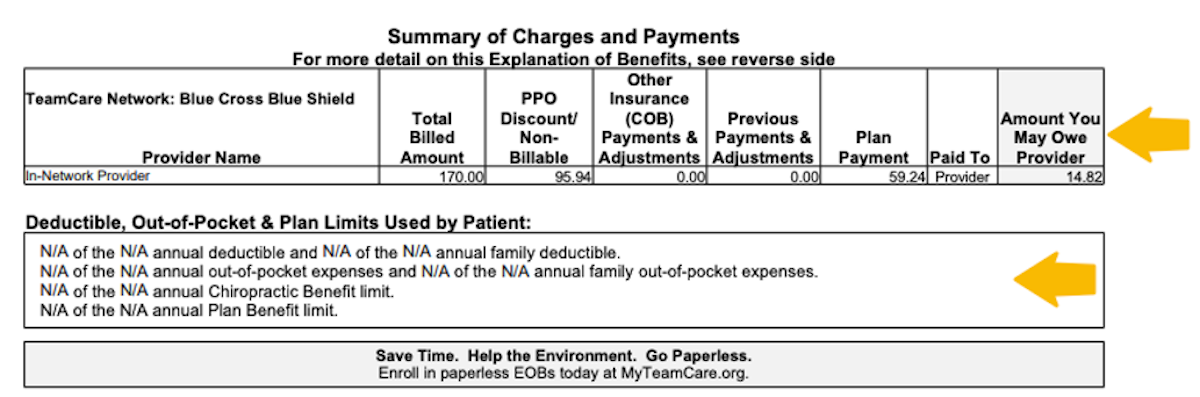
 3
3This section provides a complete breakdown of your charges. You’ll find the service dates, type of service, billed amount, allowed amount, co-pay, deductible, eligible amount, benefit rate, plan payment, co-insurance, and total you may owe.
The next two sections detail the description of type of service you or your dependents received, and any remarks related to the EOB.
-
 4
4If you suspect any billing or coverage errors, you have two ways to take action. You can contact your healthcare provider directly, or complete and submit an appeals form by mail or through the Message Center within 180 days. Learn more about How to Appeal a Claim and download an appeals form.
If you have questions, please send a secure message through the Message Center or call a Benefits Specialist at 1-800-TEAMCARE (1-800-832-6227).